(This article is based on the writing of dentist Viktoria Ljutkina, published in the largest dental medicine periodical in Estonia, Ajakiri Hambaarst. Ljutkina works as a dentist at Läänemere Hambakliinikus dental clinic in Tallinn.)
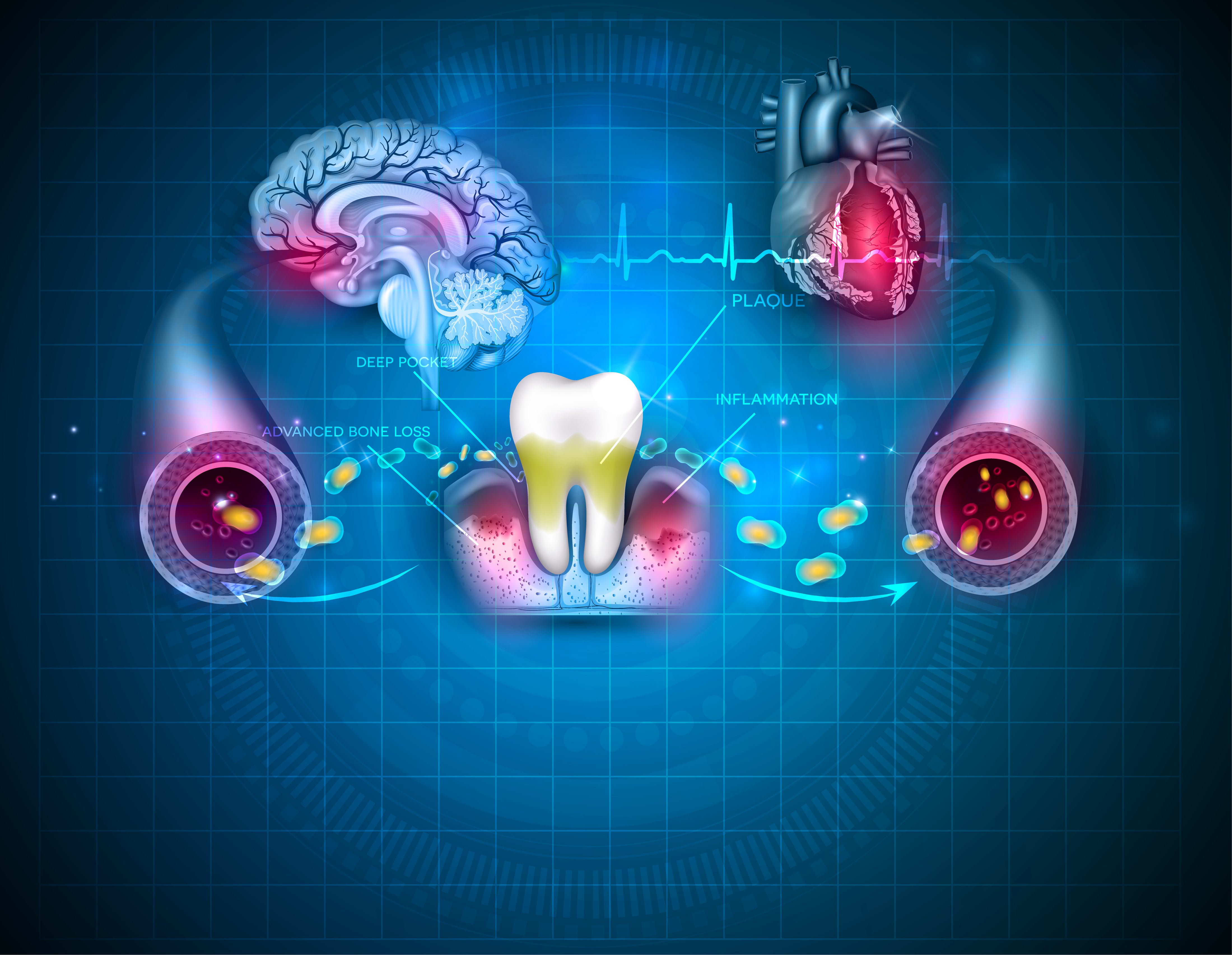
Periodontitis is a common disease affecting an estimated 20–50% of the population. This severe oral condition originates in the gum tissue, and if left untreated, the inflammatory process spreads deeper, leading to tooth loss (1). Periodontitis is a multifactorial disease primarily caused by bacterial colonization in the oral cavity (2). Many risk factors, such as diabetes and smoking, contribute to the development of periodontitis and influence its prognosis.
The goal of periodontitis treatment is to eliminate factors promoting inflammation in the oral cavity and support the patient's immune system. Fundamental to gum disease treatment is meticulous oral hygiene, preventing the formation of new dental calculus and reducing the number of bacteria in the oral cavity, thereby promoting periodontitis healing (3). The effects of Antimicrobial Photodynamic Therapy (aPDT) on oral diseases, including periodontitis and peri-implantitis, have been extensively studied, with substantial clinical evidence supporting its effectiveness.
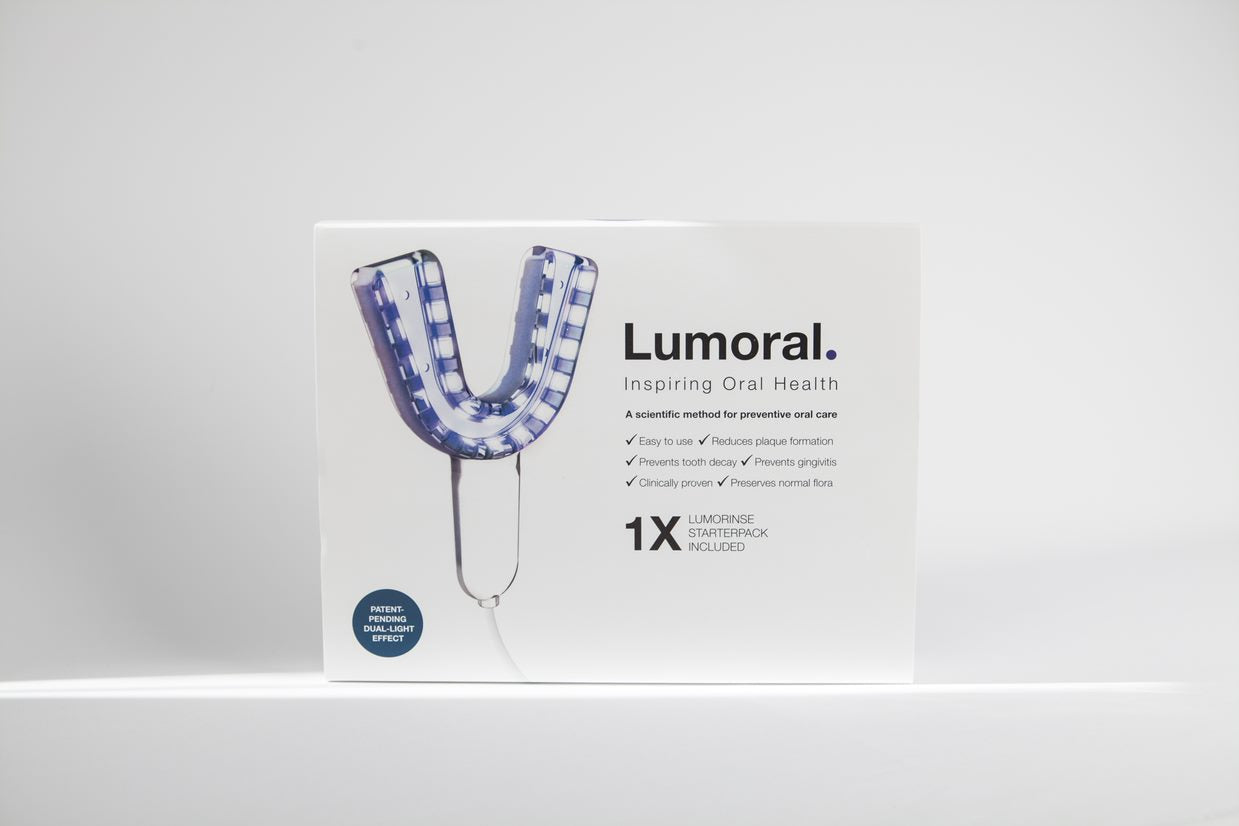
The Lumoral oral care method, developed by Finnish scientists, is based on dual-light antibacterial therapy that can be administered at home. Lumoral's effects have been scientifically proven in various clinical studies. Regular use of Lumoral prevents tooth decay and significantly reduces the count of periodontal bacteria in the mouth (4).
Lumoral treatment relies on the administration of dual-light therapy through the Lumoral oral device – near-infrared light and antibacterial blue light. The near-infrared light has a wavelength of 810 nm, penetrating tissues up to 10 cm deep. Antibacterial blue light, with a wavelength of 410 nm, acts on inflammation-causing bacteria, slowing down their growth. When porphyrin molecules in the bacteria are exposed to specific wavelengths of light, they produce reactive oxygen species, which, in turn, kill the bacteria.
Lumoral is effective against harmful bacteria in the mouth
The Lumoral method includes a light source and a mouthwash. The photosensitive indocyanine green molecule in the Lumorinse mouthwash, in combination with the light source, achieves the desired therapeutic outcome. Indocyanine green (ICG) is water-soluble and highly light-absorbing. The dual light reacts with the ICG photosensitizer, generating reactive oxygen species (ROS) and heat, initiating a series of photochemical and biological processes that destroy the bacterial cell membrane, thereby damaging the bacterial cell structure.
The body's immune cells use a similar method to protect against harmful pathogens. Pathogenic bacteria contain porphyrin and flavin molecules with photosensitive properties. Therefore, Lumoral mainly affects pathogenic bacteria.
The Lumoral method has proven to be highly effective against harmful bacteria, with no development of bacterial resistance even with repeated use (5). The largest European study on periodontitis demonstrates significant improvement in treatment outcomes when dental calculus is regularly removed from the mouth. Lumoral has been shown to help users achieve better oral hygiene, even after using the most modern and efficient electric toothbrushes, which can leave plaque on teeth. The study also indicates that Lumoral aids in achieving better oral hygiene.
In support of brushing and flossing
Lumoral does not replace the need for mechanical brushing and cleaning between teeth but helps further improve oral hygiene. Effectively, Lumoral can remove bacteria from the surfaces of teeth and even from the gumline, where access with a toothbrush may be challenging.
aPDT treatment has proven to be significantly more effective and better tolerated than commonly used chlorhexidine mouthwashes. Home use of Lumoral reduces gum inflammation and enhances oral hygiene. Effective oral hygiene also enhances the efficiency of periodontal treatment (6).
Periodontal treatment and improvement of oral hygiene are considered the gold standard in periodontitis treatment. However, some patients may not respond positively to treatment due to risk factors and/or systemic diseases.
Smoking is considered a major risk factor for gum diseases, negatively impacting both the course of the disease and treatment outcomes. Nicotine in tobacco products hinders the oral cavity's defense mechanisms, impedes the healing of periodontal tissues, and adversely affects tissue blood circulation. Changes in the oral microbiome also occur due to smoking, promoting the development of advanced periodontitis and poorer healing after treatment. Finding effective treatment for smoking patients with periodontitis is crucial because managing periodontitis based on the aforementioned biological processes poses a significant challenge for physicians (7).
Independent Lumoral study shows efficacy
I decided to try the Lumoral method at Läänemere Hambakliinikus dental clinic to improve oral hygiene in patients with periodontitis. Twelve smoking patients with generalized periodontitis at stage III, grade B, and without other chronic diseases were selected for the clinical study. Half of the patients received Lumoral photodynamic therapy 2–3 times a week for six months (recommended dose after periodontal treatment twice daily for four weeks). The remaining patients received traditional periodontal treatment only. The general treatment strategy was similar for all patients, including comprehensive diagnostics (periodontal condition, radiological diagnostics, anamnesis), non-surgical periodontal treatment, and periodontal follow-ups at two weeks, three months, and six months. During the control visits, patients' dental calculus was stained to check oral hygiene.
I noticed that patients using Lumoral in addition to traditional treatment showed better results in periodontal treatment outcomes (pocket depths, tooth mobility, BOP, VIP, SUP) and oral hygiene compared to those not using Lumoral as an oral hygiene aid. Based on my clinical experience, we can conclude that using the Lumoral method improves patients' oral hygiene and leads to more positive treatment outcomes. It is essential to use the device correctly and regularly following the dentist's recommendations.
References:
Petersen, P. E., Baehni, P. C. Periodontal health and global public health. Periodontol 2000. 2012 Oct; 60 (1): 7–14.
Bartold, P. M., Van Dyke, T. E. Periodontitis: a host-mediated disruption of microbial homeostasis. Unlearning learned concepts. Periodontol 2000. 2013 Jun; 62 (1): 203–17.
Greenstein, G. Research, Science and Therapy Committee of the American Academy of Periodontology. The Role of supra- and subgingival irrigation in the treatment of periodontal diseases. J Periodontol. 2005; 76: 2015–27.
Villafuerte, K. R., Martinez, C. J. H., Vieira, L. H. P., Nobre, A. V. Benefits of antimicrobial photodynamic therapy as an adjunct to non-surgical periodontal treatment in smokers with periodontitis: a systematic review and meta-analysis. Medicina 2023, 59 (4): 684.
Lähteenmäki, H., Pätilä, T., Räisänen, I. T., Kankuri, E., Tervahartiala, T., Sorsa, T. Repeated Homeapplied dual-light antibacterial photodynamis therapy can reduce

Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.